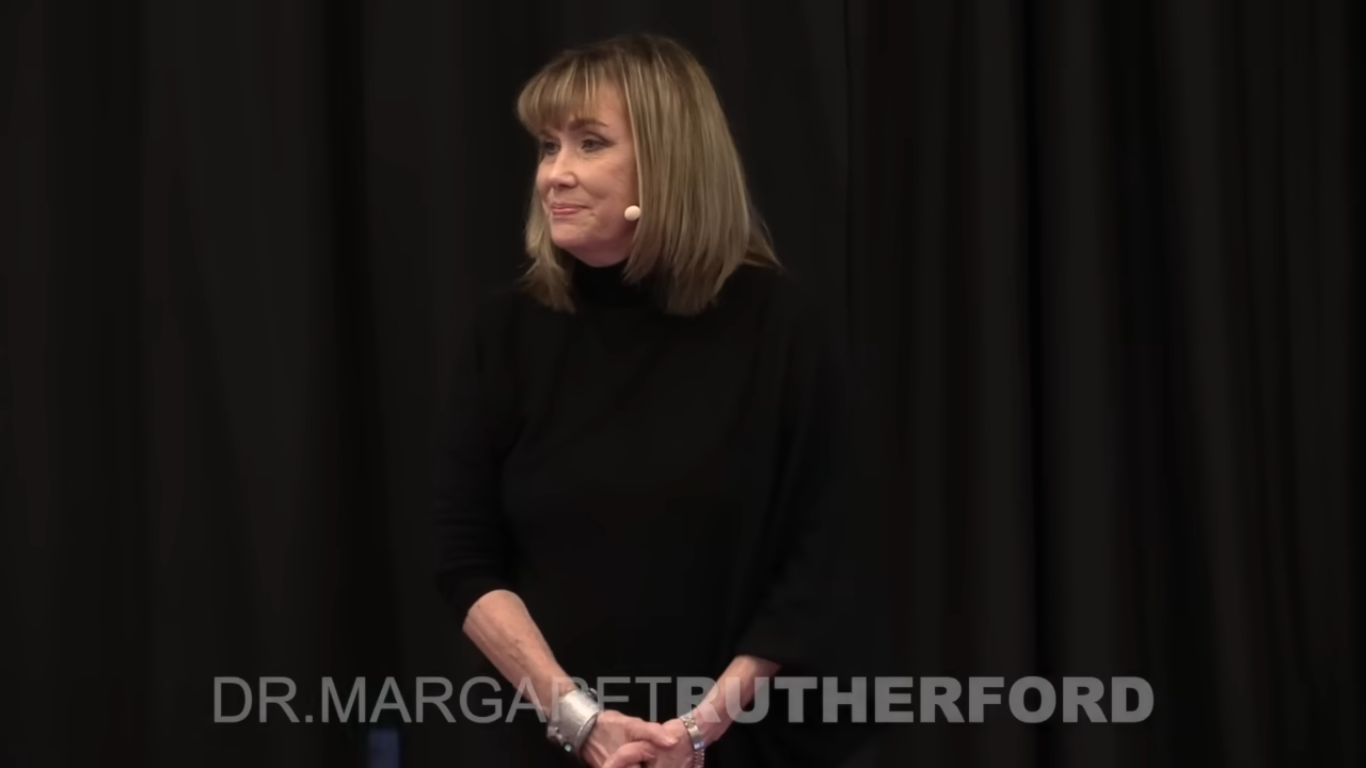
Discover the transformative insights of Dr. Margaret Rutherford on perfectly hidden depression. Learn how fostering transparency about mental health and painful secrets can lead to healing and save lives. Explore her book, “Perfectly Hidden Depression,” and her acclaimed podcast, The SelfWork Podcast, for expert advice on breaking free from perfectionism and improving mental health.
Speech:
Let me tell you about Natalie. Natalie came into therapy almost apologetically. She giggled as she told me about what sounded like panic disorder, her heart racing, and difficulty breathing. Maybe she wanted to run out of the room when she felt pressured. Otherwise, she was very successful. She had friends galore, a good marriage, and she loved her kids. She said, “My life’s almost perfect. I just need to calm down.”
I’d been a therapist for about eight years when I saw her and I thought, you know, this is a pretty common anxiety disorder. I need to help her find out what’s making her anxious and what she can do about it. But one afternoon I got a call from her husband, Jeff, and he said, “Something’s wrong. I got this weird message from Natalie asking me to pick up the kids when I get back into town and take them to her mother’s.” I thought about our last session, and nothing really strange had happened. She’d even said therapy was helping. But I heard Jeff’s tone, and my gut said differently.
So I listened to it and I drove to their home and let myself in with the garage code that Jeff had given me. I walked into the kitchen. I saw recently washed dishes and towels neatly folded by the sink. There was no sound. Just silence. I started calling Natalie’s name, hoping that she’d come around the corner, being embarrassed that she’d had another panic attack and wanting to know why and how I was getting in her house. But instead, I found her lying in bed, an empty vodka bottle, and several stray pills laying on the table.
I called 911 with her, saying, “Oh, don’t call. I’m fine.” When the paramedics rushed her out, I just stood there, stunned. I had no idea that Natalie was suicidal. None. I felt to blame and not to blame. What had I missed? What if I had listened to my gut? What if I hadn’t called Jeff back? But the fact remained. I diagnosed her with panic disorder and mild depression because that’s what Natalie had allowed me to see.
We all have secrets. And it’s not always the secrets themselves that get us into trouble, but the feelings about the secrets that can darken and deepen over time. Some of those feelings can be terror, fear, shame, self-loathing, and worse. Unfortunately, many of us learned that it’s not okay, or we’re just never taught that it’s okay to express those feelings. So we deny their existence on the outside. We’re fine. While on the inside there can be immense feelings of despair, loneliness, and hopelessness. Natalie had secrets, but it was her secret feelings that nearly killed her.
Can you imagine a world where talking about these secrets is not shameful? Is it possible to create a culture where expressing those feelings is not shameful but actually can be seen as healthy self-acceptance and even personal strength? Sixteen years and hundreds of patients later, I wrote a blog post. I was describing people like Natalie and what it might be like to live their lives day in and day out. I just wrote about successful-looking people who were hiding their struggles. I didn’t think it was particularly profound. But that post went viral because I had called it and defined it perfectly: Hidden Depression.
My email was swamped with messages from people who said, “I have these feelings and no one knows. It’s like you’re in my head.” And the more I wrote and received feedback, I began to understand how trapped people can feel in this cage of rigid emotional control with fear and shame, keeping them terrified of discovery. So I put two and two together and said, “Oh, a perfect-seeming life can serve as camouflage.” But there’s an obvious problem. How can we identify that someone needs help if they don’t tell us, feel like they can’t tell us, or don’t know how?
For example, let’s say someone like Natalie goes to make a tentative trip, maybe goes to the doctor or a clinician’s office. The professional would do what they were taught to do, which would be to assess the presence of mental illness using the Diagnostic and Statistical Manual of Mental Disorders. The DSM, as it’s called, offers internationally recognized psychiatric symptom checklists, some of which are then required to earn a certain diagnosis. This is based on the medical model of mental illness, which many believe overemphasizes the biological aspects of depression. But it becomes the lens through which that professional begins to see the problem. And certain questions are then asked that reflect those symptoms and that lens.
Does the patient report sleep and appetite disturbance? No. Has the patient lost pleasure in things they used to enjoy? No. Does the patient have foggy thinking? No, not till right now. Does the patient have suicidal thinking? No. My life is far too full of grateful things. The exact process I’d used with Natalie. The problem is the lens. Your lens determines what you see. Combine the limitations of that professional’s lens with the patient’s fear of revealing vulnerability. And my friends, we have a problem.
In 1993, the founder of the American Association of Suicidology, Edwin Schneidman, was a well-respected thought leader and researcher in the world of suicide and depression. He coined a term called “psychache,” meaning intolerable emotional and psychological pain. And his research upended common psychiatric thinking at the time because he found that psychache had more to do with suicide than depression. “Pain is at the core of suicide,” he said. Meaning that the answers to treating people with suicidal feelings does not lie in the assignment of a diagnosis, but by an acknowledgment and working through of that pain.
Two years later, Sidney Blatt, another renowned researcher, warned that when perfectionism is found alongside depression, it can drastically change depression’s presentation and must not be assessed through diagnostic measures, but through understanding the perception of that person of themselves and their world. But we are so governed by the medical model of mental illness that unless someone’s depression meets the criteria, the official DSM criteria for depression, it is likely to be missed. While suicide rates are skyrocketing worldwide, I’d wager that it will not be long before every one of us, every single one of us either know someone personally or has heard the story of someone whose life was going great, and they died by suicide.
That person, your friend, your neighbor, your kid’s soccer coach, your pastor, your professor, your work buddy, and maybe even your child is keeping their pain secret. Now, why? Again, those who identify with what I term “perfectly hidden depression” feel that they must protect themselves with this shield of silence. They’re not going to fit into the pre-assigned DSM criteria. And in fact, they are ashamed that anyone might think of them or see them as depressed.
So what can we do? How can we change or set the stage for increased transparency? I think, I know that we must recognize that suicidal feelings and the thoughts that accompany them are, believe it or not, normal. To be clear, I’m not saying that suicide is normal. I’m saying that thoughts about suicide are much more common than most of us know. I cannot count the number of people over the years who reveal such feelings to me. Sometimes hesitatingly, fearing that I’ll do something radical or take away their rights, sometimes with great relief, because they begin to let go of a shame that has literally seeped down into the very core of their being. And sometimes with sadness because they realize just how close they’ve come.
Now there are people who have the intent to die, have the means to do it, and cannot tell you why they shouldn’t. Those people tell someone like me because they want my help to keep them safe and they must be taken very seriously. But so many suicidal feelings are natural human normal responses to what has happened in your life. So why don’t we treat it as normal? Why don’t we talk about the feelings that we would talk about any other way? Why don’t we ask? “Well, when do you feel this? When do you not feel this? What’s it like to talk to me about it? Have you ever wondered what would make it go away?” Questions that we would ask about any other feelings that a person was trying to understand and cope with.
But these are not questions about symptom criteria. We are going to go in the direction that John Sommers-Flanagan wants us to go, which is working toward a strength-based assessment of suicide. Now what does this have to do with you? You’re probably not a clinician or a doctor. How would you respond if someone told you they were thinking about taking their own life? Sadly, the instinct is often, “I can’t believe you said that. You know, you have people who love you. How can you be so selfish?” And the quickest way to end a conversation is to blame someone for the way they’re feeling or to suggest that no one that was literally loving and caring would ever have that feeling.
What if instead we could approach not with judgment, but with acceptance? Many more conversations will take place. Let me tell you about Michael. Michael was an internationally prominent person in his field when he came to see me, and he was laughing because he said, “No one would ever imagine me going to therapy.” He’d grown up in a family where they didn’t discuss feelings, especially painful ones. But his father had died suddenly, and Michael had never told his dad that he loved him, despite the tumultuous relationship they’d had. And Michael couldn’t forgive himself for that.
As we talked about his childhood and current decisions he was trying to make, he began to see patterns. He could see how he’d covered up his horrific abuse as a child and tried to cover it up with greater and greater achievement to reach some sort of destination that would blot out or blur the painful secrets he kept hidden inside. But it didn’t work. He told me one day, very painfully, that he also had feelings of
the intent to die. I told him those feelings were normal, given the extent of his pain and how long he had felt it. In our continuing work, he found that he could have compassion for himself without carrying the shame that was not his to carry. He could grieve without pummeling himself with self-loathing, and he could decide to live.
I truly will never forget the day that Michael strolled into my office, laughing, a big smile on his face and said, “Hey, doc, I got to tell you something. I was on this crowded airplane journaling instead of working. Writing about my childhood and my father in public. And when I felt a tear rolled down my cheek. I didn’t care.”
We all have secrets, but the cost that can accompany the feelings of those secrets has never been more evident. You and I can realize we can have an impact right now on our culture so that transparency is seen as strength. Thank you.


Leave A Comment